The first time I witnessed a generative AI system accurately synthesize a patient’s complex medical history into actionable clinical insights, I understood we were entering a new era of healthcare delivery. After two decades of architecting enterprise systems across industries, I can say that healthcare presents both the greatest challenges and the most profound opportunities for AI transformation. The stakes are higher—we are dealing with human lives—but the potential to improve outcomes, reduce costs, and expand access to quality care makes this work essential.
The Healthcare Data Foundation
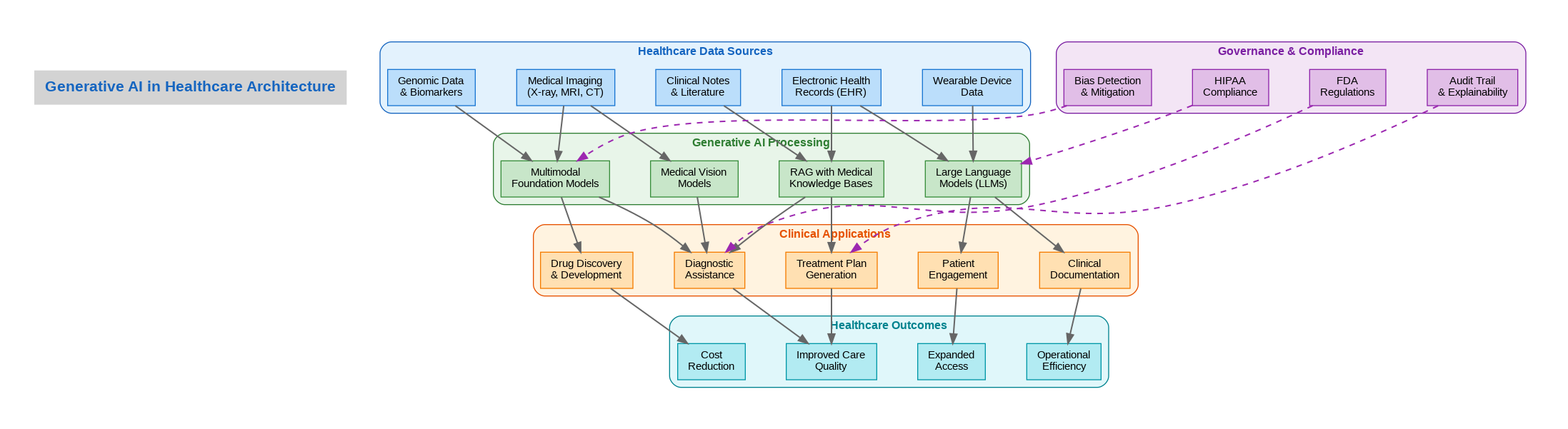
Healthcare generates staggering volumes of data: electronic health records containing decades of patient histories, medical imaging from X-rays to MRIs, genomic sequences, wearable device streams, and unstructured clinical notes written by physicians. The challenge has never been data availability but rather the ability to synthesize this information into timely, actionable insights. Generative AI changes this equation fundamentally by processing multimodal data at scales impossible for human clinicians while maintaining the contextual understanding necessary for medical decision-making.
In production deployments I have architected, the integration of large language models with retrieval-augmented generation (RAG) systems connected to medical knowledge bases has proven transformative. Rather than relying solely on model training data, these systems ground their responses in current medical literature, drug interaction databases, and clinical guidelines. This approach addresses one of the critical concerns in healthcare AI: the need for responses that reflect the latest medical evidence rather than potentially outdated training data.
Clinical Applications Transforming Care
Diagnostic assistance represents one of the most impactful applications. Medical vision models trained on millions of imaging studies can detect patterns that escape human observation—early-stage tumors in mammograms, subtle fractures in X-rays, or diabetic retinopathy indicators in fundus photographs. In radiology departments where I have implemented these systems, the AI serves as a second reader, flagging potential findings for radiologist review rather than replacing clinical judgment. This human-in-the-loop approach maintains physician oversight while dramatically improving detection rates.
Clinical documentation consumes an enormous portion of physician time—studies suggest doctors spend two hours on paperwork for every hour of patient care. Generative AI transforms this burden by automatically generating discharge summaries, progress notes, and referral letters from structured data and voice recordings. The physician reviews and approves the generated content rather than creating it from scratch, reclaiming hours that can be redirected to patient interaction.
Treatment plan generation leverages the AI’s ability to synthesize patient-specific factors with evidence-based guidelines. For complex cases involving multiple comorbidities and potential drug interactions, the system can propose treatment options ranked by expected efficacy, contraindication risks, and cost considerations. Oncology departments have found particular value in these capabilities, where treatment decisions must balance tumor characteristics, patient health status, and rapidly evolving therapeutic options.
Governance and Regulatory Considerations
Healthcare AI operates within one of the most heavily regulated environments in technology. HIPAA compliance in the United States, GDPR in Europe, and similar frameworks globally impose strict requirements on patient data handling. Every AI system I have deployed in healthcare includes comprehensive audit trails capturing inputs, outputs, and the reasoning chains that led to recommendations. This explainability is not merely a technical feature but a regulatory requirement and an ethical imperative.
Bias detection and mitigation deserve particular attention. Training data reflecting historical healthcare disparities can perpetuate or amplify inequities in AI recommendations. Production systems must include continuous monitoring for differential performance across demographic groups, with mechanisms to identify and correct biased outputs before they affect patient care. FDA guidance on AI-based medical devices increasingly emphasizes these fairness considerations alongside traditional safety and efficacy requirements.
Implementation Lessons from Production
Successful healthcare AI deployment requires deep integration with existing clinical workflows. Systems that require physicians to leave their electronic health record interface to access AI capabilities see minimal adoption regardless of their technical sophistication. The most effective implementations embed AI assistance directly within the tools clinicians already use, presenting recommendations at the moment of decision-making rather than requiring separate consultation.
Change management proves as important as technical implementation. Clinicians understandably approach AI recommendations with skepticism, particularly when the systems cannot explain their reasoning. Building trust requires transparency about model capabilities and limitations, clear communication about the AI’s role as an assistant rather than a replacement, and demonstrated value through improved patient outcomes. Organizations that invest in clinician education and feedback mechanisms see dramatically higher adoption rates than those focused solely on technical deployment.
The transformation of healthcare through generative AI is not a future possibility but a present reality. Organizations that approach this transformation thoughtfully—balancing innovation with safety, efficiency with equity, and automation with human oversight—will define the standard of care for the coming decades. The technology is ready; the challenge now is implementation that honors both the promise and the responsibility of healthcare delivery.
Discover more from C4: Container, Code, Cloud & Context
Subscribe to get the latest posts sent to your email.
